A Guide to Root Canal Treatment: What to Do?
Ömer ÖZKOCA2025-08-01T12:32:12+03:00Root canal treatment is a critical dental procedure that can save a severely infected or damaged tooth — helping you avoid extraction and preserve your natural smile. It involves removing diseased pulp from within the tooth, cleaning and disinfecting the root canals, and sealing the space to prevent reinfection. While some may feel anxious about the process, modern techniques and anesthesia now make root canal treatments much more comfortable and efficient. In this guide, we’ll walk you through what a root canal treatment is, who needs it, how it’s done, and why timely care matters.
Table of Contents
ToggleWhat Is Root Canal Treatment and Do You Need It?
Root canal treatment (also known as endodontic therapy) becomes necessary when the pulp—the soft tissue inside a tooth—becomes inflamed or infected. This can happen due to deep decay, repeated dental procedures, cracks or chips in the tooth, or trauma. Without treatment, the infection can cause severe pain or lead to abscess formation and potential tooth loss.
Key symptoms indicating the need for root canal treatment include lingering sensitivity to hot or cold, swelling or tenderness of nearby gums, and pain when chewing or applying pressure. For some people, a tooth may darken or show signs of decay without pain — yet X‑rays reveal decay approaching the root. A dentist will examine clinical symptoms, conduct dental tests, and take X‑rays to determine if root canal treatment is the best option to save the tooth.
Skipping treatment can lead to worsening infection, further decay, and often extraction. Root canal treatment aims to remove the infected tissue while preserving the remaining tooth structure. Once complete, the tooth is typically restored with a crown or filling to provide strength and functionality for years to come.
Root Canal Treatment Procedure: What to Expect During and After
When undergoing root canal treatment, you can expect a structured, multi-stage process. First, your dentist or endodontist will numb the area using local anesthesia to ensure the procedure is pain-free. A small rubber dam will isolate the tooth and keep it dry during treatment.
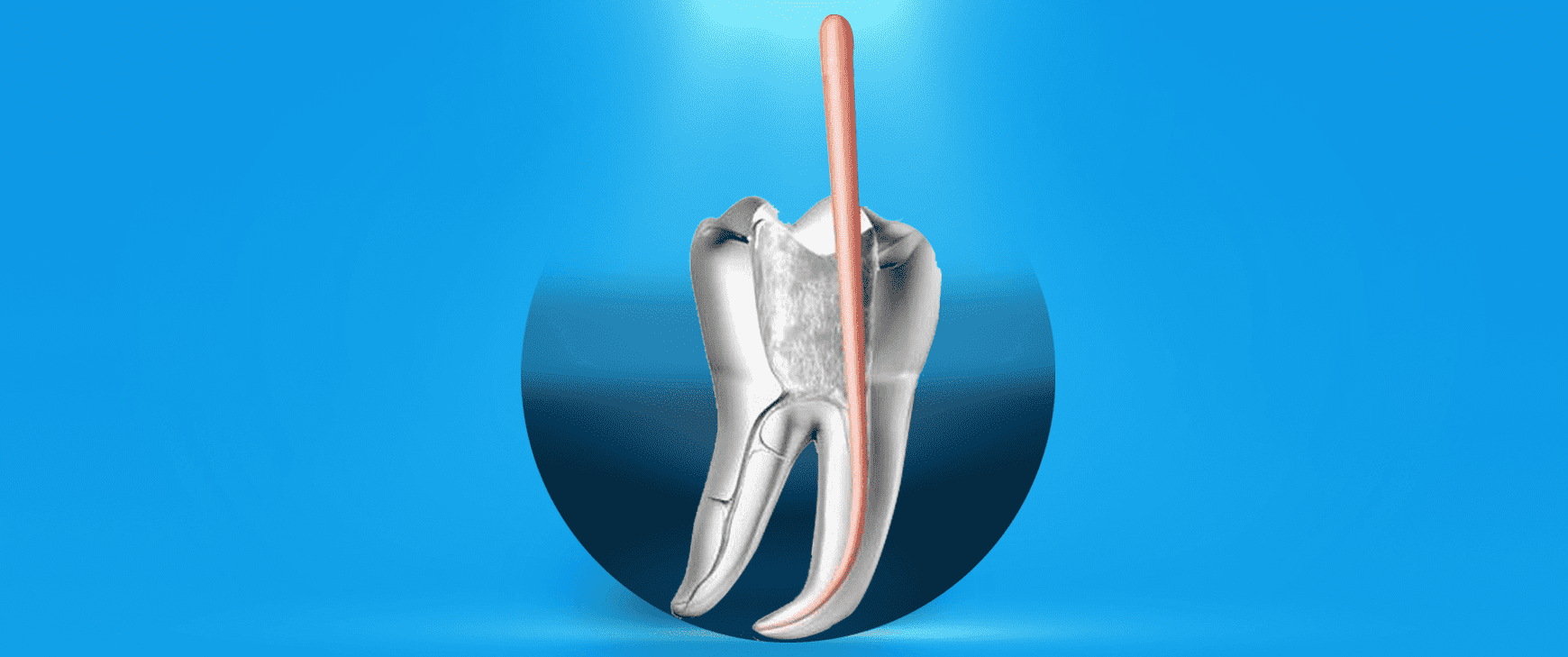
Next, the pulp chamber is accessed through a small opening in the crown of the tooth. Instruments are used to carefully remove infected pulp and shape the canals. These canals are thoroughly cleaned, disinfected, and filled with biocompatible material (usually gutta-percha) to seal the space and prevent reinfection.
A temporary filling may be placed initially, and the definitive restoration—often a dental crown—is installed in a follow-up visit. Crowns restore function and protect the tooth from fracture. Recovery is typically smooth; most patients resume normal activities within a day or two. Mild sensitivity or soreness can occur post-procedure but usually subsides in a few days.
Good aftercare—including avoiding very hard foods immediately post‑treatment and maintaining oral hygiene—ensures optimal healing and long-term success.
Does Root Canal Treatment Hurt? Dispelling the Myths
Many patients worry that root canal treatment will be painful. However, the reality is quite different: modern anesthesia and techniques have significantly improved patient comfort. Before beginning, the area is numbed, making the procedure pain-free.
During treatment, you should feel pressure but no sharp pain. If you experience discomfort at any point, the dental team will adjust anesthesia. The procedure is intended to relieve pain caused by the infected pulp, so most people leave feeling better than when they arrived. In rare cases, residual soreness may continue for several days, especially if infection was advanced.
Post‑procedure pain can be managed effectively with over‑the‑counter pain relievers, as advised by your dentist. Any persistent or severe pain should be reported promptly, as it may indicate reinfection or complications. With proper care and follow‑up, root canal treatment should bring relief, not prolong discomfort.
How Long Does Root Canal Treatment Take? Timing & Appointments
The duration of root canal treatment varies depending on the complexity of the case. For a front tooth with a single canal, one appointment may suffice. For premolars or molars with multiple roots, teeth often requiring two visits: one to clean and shape the canals, then another to finalize filling and restoration.
Each appointment generally lasts between 60 and 90 minutes. Complicated cases—such as retreatment or severely curved canals—can take longer. Scheduling also depends on whether a crown is needed immediately after or on a separate visit.
Patients should plan for some downtime: avoid chewing on the treated side until numbness wears off, and choose comfortable foods in the days following treatment. Following your dentist’s timing recommendations ensures proper healing and optimal results.
What Causes a Tooth to Require Endodontic Therapy?
Root canal treatment becomes necessary when the pulp inside a tooth becomes infected, inflamed, or damaged. The pulp, which contains nerves and blood vessels, plays a vital role during tooth development but becomes less essential once the tooth is fully mature. However, it remains vulnerable to trauma, infection, and decay.
The most common cause of root canal treatment is deep tooth decay that extends beyond the enamel and dentin, reaching the pulp. Bacteria invade the inner chamber, leading to inflammation and infection. Repeated dental procedures on the same tooth—such as multiple fillings or restorations—can also stress the pulp tissue. In some cases, a tooth that suffers a crack or fracture may expose the pulp to bacteria.
Trauma, even when it doesn’t cause visible damage, can disrupt blood flow within the tooth and lead to pulp death over time. Teeth that suddenly discolor may be showing signs of internal breakdown.
If pulp damage is not treated, it can result in severe pain, abscesses, and even bone loss around the roots. In such cases, root canal treatment is the only way to eliminate the infection while preserving the natural tooth structure. Early intervention prevents complications and often leads to a more predictable outcome.
How Much Does Root Canal Treatment Cost? Factors That Affect Your Bill
The cost of root canal treatment varies depending on several clinical and logistical factors. There is no universal price, as treatment complexity, tooth location, and geographic region all influence what you’ll pay.
Posterior teeth like molars typically have multiple canals and are more complex to treat than front teeth, which have fewer roots. This makes molar treatment more expensive due to increased chair time and technical difficulty. Similarly, if an endodontist—a root canal specialist—is involved, the cost may be higher compared to general dentistry, but the precision can enhance success rates.
Another factor is the need for diagnostic imaging like CBCT scans, which help evaluate root shape and surrounding bone. Additionally, the final restoration after the procedure, such as a dental crown, is often billed separately and adds to the total cost.
Geography matters too. Treatment in metropolitan areas tends to be priced higher due to overhead and demand. Dental insurance may cover a portion of the cost, depending on your plan and whether the tooth is being saved for medical necessity or cosmetic reasons.
To understand what your root canal treatment may cost, consult your provider for a full evaluation. A detailed estimate can be created once the diagnosis and treatment plan are finalized.
5 Crucial Questions to Ask About Your Root Canal Procedure

Before undergoing root canal treatment, it’s helpful to ask your dentist a few essential questions to understand the procedure and feel confident in your care. Knowing what to expect reduces anxiety and ensures you make informed decisions.
Why do I need this treatment? This clarifies whether the pulp is infected, damaged, or inflamed and confirms whether the treatment is necessary for tooth preservation.
What are my alternatives? In some cases, extraction or waiting may be presented as alternatives, but saving the natural tooth is usually preferred if viable.
What type of restoration will I need afterward? Most root canal treated teeth require a crown for protection and longevity. Understanding this helps you plan for the complete cost and timeline.
How many visits will the treatment take? Some procedures can be done in one appointment, while others may require two or more, especially if complications or infection are present.
What aftercare is required? Knowing how to care for your tooth post-treatment is crucial to avoiding complications and ensuring full healing.
Asking these questions encourages open communication with your dental provider and helps tailor the root canal treatment to your specific needs.
Role of CBCT and X-Rays in Root Canal Diagnosis and Planning
Advanced imaging is critical for successful root canal treatment. Two essential tools used during diagnosis and treatment planning are periapical X-rays and Cone Beam Computed Tomography (CBCT). These technologies help dentists visualize the internal structure of the tooth and detect hidden issues.
Periapical X-rays provide a two-dimensional view and are typically the first step in assessing root structure, infection, and bone condition. They help identify root length, canal shape, and possible fractures. However, in complex cases—such as previously treated teeth or unusual anatomy—CBCT imaging is invaluable.
CBCT produces a detailed three-dimensional image of the tooth and surrounding tissues. It allows for more accurate measurements, detects extra canals, and reveals lesions or cysts not visible on standard X-rays. This is especially useful in molars, which often have multiple, curved, or hidden canals.
With CBCT, root canal treatment becomes more precise. Dentists can navigate complex anatomy, reduce the risk of missing a canal, and plan the procedure with confidence. The result is fewer complications and higher long-term success rates.
Patients benefit from faster diagnosis and better-informed treatment, which leads to improved outcomes and reduced need for retreatment.
Why Seeing an Endodontist Might Be Better for Complex Root Canal Treatment
While many general dentists perform root canal treatment, certain cases are better handled by an endodontist—a specialist in diagnosing and treating problems within the dental pulp. These professionals undergo additional training and use specialized tools to manage complex situations.
Endodontists are particularly valuable when treating molars with multiple roots or curved canals. They are skilled at identifying unusual anatomy and have access to high-magnification microscopes and digital imaging tools, such as CBCT. This allows for more precise cleaning and filling of the canals.
Patients may be referred to an endodontist if previous treatment has failed, if pain persists without visible decay, or if the canal structure is unusually narrow. Additionally, endodontists are more experienced in procedures like root canal retreatment and apicoectomy (root-end surgery), which may be necessary when traditional treatment isn’t enough.
Choosing an endodontist for root canal treatment may result in fewer complications, a higher success rate, and potentially faster recovery. While the cost may be slightly higher, the improved precision and reduced risk of failure can justify the investment in complex cases.
Root Canal Treatment vs. Extraction: Why Saving Your Tooth Matters
When faced with a damaged or infected tooth, patients often ask whether they should choose root canal treatment or opt for extraction. While both procedures address the immediate issue, the long-term impact on oral health can be significantly different.
Root canal treatment preserves the natural tooth by removing the infected pulp, cleaning the canal system, and sealing the space. This maintains the integrity of your bite, keeps surrounding teeth in position, and helps prevent bone loss in the jaw. Retaining the natural tooth also makes eating and speaking more comfortable compared to a gap or removable prosthetic.
Tooth extraction may seem like a quicker solution, but it introduces its own set of challenges. After removal, adjacent teeth may shift, leading to misalignment or bite problems. Bone loss at the extraction site is also common, and replacement with implants or bridges requires additional time, cost, and procedures.
Most dentists recommend root canal treatment whenever possible, as it offers a more conservative, long-term solution. While extraction may be necessary if the tooth is too damaged to repair, saving a natural tooth generally yields better results for function, aesthetics, and cost-efficiency in the long run.
Retreatment or Root Canal Surgery: When Initial Treatment Isn’t Enough
In some cases, root canal treatment may not completely resolve the infection or the tooth may become reinfected years later. When this occurs, retreatment or surgical alternatives like apicoectomy may be needed to preserve the tooth.
Retreatment involves reopening the tooth, removing the original filling material, cleaning the canals again, and resealing them. This is typically recommended when a canal was missed during the first procedure, if the filling material did not seal properly, or if new decay has affected the tooth. Technological advances such as dental microscopes and CBCT imaging significantly improve the chances of success in retreatment.
If retreatment is not feasible due to structural complications or persistent infection near the root tip, an apicoectomy may be considered. This minor surgical procedure removes the tip of the root and any surrounding infected tissue.
Both retreatment and surgery aim to avoid tooth extraction. Your dentist or endodontist will evaluate the cause of failure and recommend the most appropriate approach. Even when the first root canal treatment does not succeed, these secondary options can help maintain the natural tooth for many more years.
Common Complications of Root Canal Treatment and How to Prevent Them

Although root canal treatment has a high success rate, complications can occur. Understanding these risks and how to prevent them helps patients achieve better outcomes.
One potential issue is a missed canal. Some teeth have extra or unusually shaped canals that may not be detected with standard X-rays. If untreated, these canals can harbor bacteria and lead to reinfection. Advanced imaging and magnification tools significantly reduce this risk.
Instrument separation is another complication, where a small file used to clean the canals breaks off inside the tooth. While often harmless, in some cases it may require additional intervention. Ensuring that an experienced provider performs the procedure can help minimize these occurrences.
Post-treatment pain or swelling is usually temporary but may indicate persistent infection or inflammation. In such cases, follow-up treatment or retreatment may be needed.
To avoid complications, follow your dentist’s post-operative instructions closely. Maintain excellent oral hygiene, attend follow-up appointments, and avoid chewing hard foods on the treated tooth until fully restored.
With proper technique and care, most root canal treatments are successful and long-lasting.
Restoring a Root Canal Treated Tooth: Crowns, Fillings, and More
After root canal treatment, the next essential step is restoring the tooth to protect it and restore full function. The restoration method depends on the tooth’s location, how much structure remains, and the level of bite force it endures.
Posterior teeth, such as molars and premolars, often require dental crowns because they handle most of the chewing forces. A crown encases the entire tooth, reinforcing its structure and reducing the risk of fracture. This is especially important because root canal-treated teeth can become more brittle over time.
Anterior teeth may only need a composite filling or a partial crown if enough natural structure remains. However, aesthetics and alignment still play a role in deciding the final restoration.
Delaying the restoration can expose the tooth to bacterial contamination and structural damage. That’s why most dentists recommend placing a permanent restoration within a few weeks after completing root canal treatment.
Discussing restoration options early ensures the final outcome looks natural, feels comfortable, and lasts for years.
It might interest you –> Dental Bone Graft
Root Canal Infection and Abscess Risks: What You Should Know
A major reason for root canal treatment is to prevent or treat a dental abscess—an accumulation of pus caused by bacterial infection. If left untreated, a deep cavity or cracked tooth can allow bacteria to reach the pulp and spread through the root canals into surrounding tissues.
This can result in swelling, severe pain, bad taste, fever, and even facial swelling. In more advanced cases, the infection can spread to other parts of the body, making early diagnosis and treatment essential.
Root canal treatment removes the source of infection, disinfects the internal structure of the tooth, and prevents bacteria from re-entering. However, if the infection is extensive or the procedure is delayed, pus can accumulate at the tip of the root and form an abscess. In some cases, draining the area or performing an apicoectomy may be necessary.
Good oral hygiene and routine check-ups reduce the risk of infection. If you notice throbbing pain, swelling, or a pimple-like bump on the gums, seek dental care promptly. Early root canal treatment can prevent these risks and help preserve your natural tooth.
For your information –> Dental Implants Turkey
Root Canal Treatment Aftercare: Tips to Protect Your Tooth Long‑Term
Root canal treatment is only the beginning of preserving a tooth that’s been compromised by infection or damage. To ensure the tooth remains healthy and functional for years to come, proper aftercare is essential.
Immediately after the procedure, patients may experience minor soreness or sensitivity, particularly if there was significant inflammation beforehand. Over-the-counter pain relievers are usually sufficient, but always follow your dentist’s guidance regarding medication. It’s important to avoid chewing on the treated side until the tooth has been permanently restored, especially if only a temporary filling is in place.
Long-term care involves excellent oral hygiene. Brush at least twice a day using fluoride toothpaste and floss daily, including around the treated tooth and any adjacent restorations. Special tools like interdental brushes or water flossers can help clean tight areas and prevent plaque buildup.
Attending routine dental check-ups is also crucial. Your dentist will monitor the treated tooth for signs of reinfection, assess the condition of the crown or filling, and ensure the surrounding gums and bone remain healthy. If any discomfort returns—such as sensitivity to pressure or recurring pain—prompt evaluation is recommended.
Diet also plays a role in longevity. Avoid habits like chewing ice, biting pens, or grinding teeth. If you clench your jaw or grind at night, wearing a custom night guard may be advised to protect both natural teeth and restorations.
With consistent care and regular professional oversight, a tooth treated with root canal therapy can remain strong and trouble-free for decades.
Click and learn –> Dental Bridge
Treatment Summary
Number of Transactions
2-3
Return to Work Process
Now
Processing Time
10 Days
Full Recovery Process
Now
Anesthesia Method
Local anesthesia
Persistence of Results
5 Years
Sensitivity Process
Non
Eating - Drinking Process
2 Hours Later
Note: *The information and recommendations on this page are for informational purposes only. Please consult your doctor for diagnosis and treatment. WhatsApp line.
Bütün İşimiz Diş